Quiz-summary
0 of 6 questions completed
Questions:
- 1
- 2
- 3
- 4
- 5
- 6
Information
Course Directors: Andrea J. Weiss, MD and David Myland Kaufman, MD
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 6 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- Answered
- Review
-
Question 1 of 6
1. Question
1 pointsThe family of a 75-year-old retired physician solicits a psychiatric consultation because she has begun to have visual hallucinations that agitate and confuse her. During the periods of hallucinations, which consist of different but familiar scenes and people, she remains fully alert, lucid, and aware that they are not “real.” The problem began several months before, following unsuccessful ocular surgery that left her blind. She is fully aware of her loss of sight, makes allowances for it, and has no cognitive impairment. Which is the most likely explanation for the patient’s hallucinations?
Correct
In keeping with the general rule that sensory deprivation leads to hallucinations, blindness leads to visual hallucinations. The Charles Bonnet syndrome, a classic neuropsychiatric disorder, consists of visual hallucinations provoked by the onset of blindness from either ocular or occipital injury. Visual hallucinations may occur only in the “blind field” of patients with homonymous hemianopsia as well as in the entire field of vision of individuals who are completely blind. Anton syndrome, another neuropsychiatric disorder, consists of denial of blindness and usually involves patients confabulating and acting as though their sight were normal. This patient’s hallucinations are probably not seizures because they differ from episode to episode. In addition, they are probably not partial complex seizures because her level consciousness remains intact.
Incorrect
In keeping with the general rule that sensory deprivation leads to hallucinations, blindness leads to visual hallucinations. The Charles Bonnet syndrome, a classic neuropsychiatric disorder, consists of visual hallucinations provoked by the onset of blindness from either ocular or occipital injury. Visual hallucinations may occur only in the “blind field” of patients with homonymous hemianopsia as well as in the entire field of vision of individuals who are completely blind. Anton syndrome, another neuropsychiatric disorder, consists of denial of blindness and usually involves patients confabulating and acting as though their sight were normal. This patient’s hallucinations are probably not seizures because they differ from episode to episode. In addition, they are probably not partial complex seizures because her level consciousness remains intact.
-
Question 2 of 6
2. Question
1 pointsIn the patient described in the previous question, after nonpharmacologic methods did not suppress the hallucinations, which medication or category of medication should the psychiatrist prescribe?
Correct
Small doses of an antipsychotic will usually suppress these hallucinations. The other medications will not help except to sedate her or make her oblivious to the hallucinations.
Incorrect
Small doses of an antipsychotic will usually suppress these hallucinations. The other medications will not help except to sedate her or make her oblivious to the hallucinations.
-
Question 3 of 6
3. Question
1 points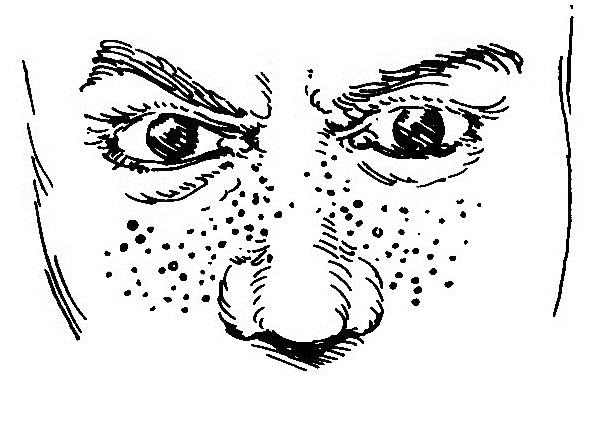
The school psychologist refers the 9-year-old student in this sketch for a psychiatric examination. The boy, who has had epilepsy for several years, has begun to slip in his interpersonal skills, language ability, and academic aptitude. Moreover, he has begun a rocking movement in class. Which is the most likely diagnosis?Correct
Although antiepileptic drugs might impair his cognitive abilities and interpersonal skills, the combination of facial adenomata, epilepsy, and autistic symptoms indicate that tuberous sclerosis is the most likely diagnosis. A CT of his head and genetic testing would prove it. Fragile X, Angelman, and Rett syndromes as well as tuberous sclerosis produce symptoms of autism.
Incorrect
Although antiepileptic drugs might impair his cognitive abilities and interpersonal skills, the combination of facial adenomata, epilepsy, and autistic symptoms indicate that tuberous sclerosis is the most likely diagnosis. A CT of his head and genetic testing would prove it. Fragile X, Angelman, and Rett syndromes as well as tuberous sclerosis produce symptoms of autism.
-
Question 4 of 6
4. Question
1 pointsA 70-year-old retired police officer, who has had Parkinson disease for 12 years, had hallucinations, paranoid ideation, and physical agitation. In conjunction with a psychiatrist, the neurologist reduced his Parkinson medication regimen; however, that change and similar strategies eliminated the psychosis but left him rigid and immobile. During the day, he had numerous periods of being “on” and, more frequently, “off.” Which therapy should the neurologist suggest?
Correct
DBS has been a major advance in treatment of Parkinson disease, dystonia, and essential tremor. Used in Parkinson disease, DBS enhances “on” periods and allows a reduction of the medications, which reduces iatrogenic psychosis. If depression had been present and unresponsive to conventional antidepressants, ECT would improve the patient’s mood and reverse his rigidity and bradykinesia.
Incorrect
DBS has been a major advance in treatment of Parkinson disease, dystonia, and essential tremor. Used in Parkinson disease, DBS enhances “on” periods and allows a reduction of the medications, which reduces iatrogenic psychosis. If depression had been present and unresponsive to conventional antidepressants, ECT would improve the patient’s mood and reverse his rigidity and bradykinesia.
-
Question 5 of 6
5. Question
1 pointsThe wife of a 65-year-old retired screen actor brings him for a consultation because he has developed cognitive impairment and occasional daytime visual hallucinations. Sometimes during sleep he swings his arms as though he were boxing. If she wakes him during these movements, he explains that has been dreaming that he is defending them from attack. He has no personal or family history of neurologic or psychiatric illness, use of medications or illicit drugs, systemic symptoms, or exposure to HIV risk factors. Neurologic examination reveals that he has a flat affect, moderate cognitive impairment, rigidity, and bradykinesia. Of the following, which is the most likely cause of his illness?
Correct
Parkinsonism accompanying the onset of dementia indicates that the underlying problem is dementia with Lewy bodies. The occasional daytime visual hallucinations and the nocturnal flailing, which is probably REM behavior disorder, are also characteristic of this illness. This situation is not Parkinson disease because dementia is a relatively late complication of that illness. Dementia is almost never one of its presenting features. This situation also does not indicate Alzheimer disease because he presents with motor impairments. He does not have delirium because he has been lucid and has no autonomic symptoms or signs.
Incorrect
Parkinsonism accompanying the onset of dementia indicates that the underlying problem is dementia with Lewy bodies. The occasional daytime visual hallucinations and the nocturnal flailing, which is probably REM behavior disorder, are also characteristic of this illness. This situation is not Parkinson disease because dementia is a relatively late complication of that illness. Dementia is almost never one of its presenting features. This situation also does not indicate Alzheimer disease because he presents with motor impairments. He does not have delirium because he has been lucid and has no autonomic symptoms or signs.
-
Question 6 of 6
6. Question
1 pointsIn the preceding case, which is the most likely neuropathology?
Correct
Accumulation of alpha-synuclein characterize dementia with Lewy bodies and Parkinson disease. Beta-amyloid deposits from plaques in Alzheimer disease. Tau accumulates in frontotemporal dementia. Multiple small cerebral infarcts cause vascular dementia.
Incorrect
Accumulation of alpha-synuclein characterize dementia with Lewy bodies and Parkinson disease. Beta-amyloid deposits from plaques in Alzheimer disease. Tau accumulates in frontotemporal dementia. Multiple small cerebral infarcts cause vascular dementia.